REVENUE NAVIGATOR
OUR POWERFUL DENIAL MANAGEMENT SOLUTION IDENTIFIES, ANALYZES, AND RESOLVES DENIED CLAIMS WITH PRECISION, UNCOVERING HIDDEN REVENUE OPPORTUNITIES ACROSS YOUR ENTIRE REVENUE CYCLE.
Combat Denials with revenue navigator
Revenue Navigator is our powerful denial management solution designed to help healthcare organizations take control of their revenue cycle. By identifying, analyzing, and resolving denied claims with precision, Revenue Navigator uncovers hidden revenue opportunities and helps prevent future losses.
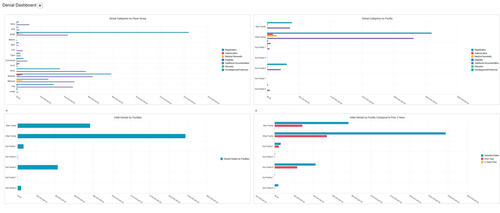
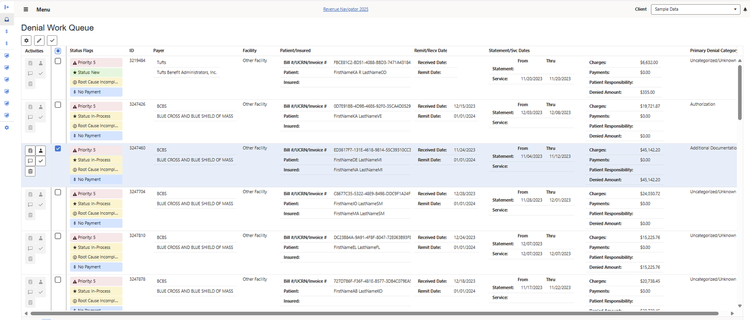
With intuitive dashboards, real-time denial tracking, and built-in trend analysis, organizations can recover hundreds of thousands of dollars annually—while streamlining workflows and improving payer performance.
Stop leaving money on the table. Start navigating your way to stronger revenue performance with Revenue Navigator.
DENIAL MANAGEMENT SOLUTION
Challenge: $20 Billion Annual Denial Crisis
Solution: Revenue Navigator Platform
Impact: Hundreds of Thousands Recovered
A comprehensive denial management platform that efficiently identifies, analyzes, and resolves denied claims. Medical denials have surged to $20 billion annually, representing massive lost revenue opportunities that can significantly impact your organization's financial health.
Revenue Navigator not only recovers lost revenue but provides actionable insights to help negotiate better contracts with insurance providers based on denial patterns, while maintaining seamless operational efficiency.
REAL-TIME ANALYTICS & TRACKING
Platform: Intuitive Dashboard System
Features: AI-Powered Insights
Integration: MRSAuditQ Compatible
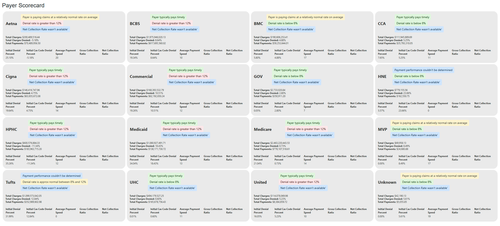
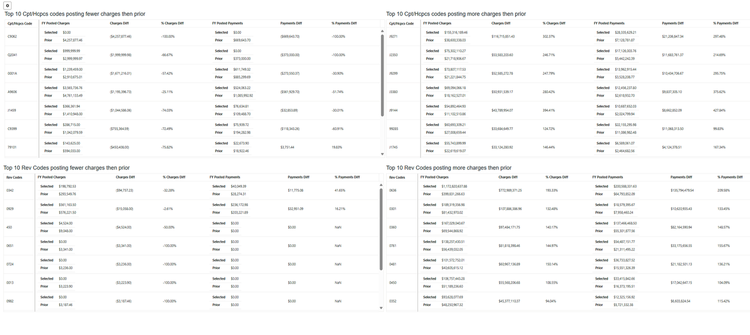
Monitor payer performance and payment accuracy with intuitive dashboards and real-time denial tracking. Our built-in trend analysis helps organizations recover hundreds of thousands of dollars annually while streamlining workflows and improving payer relationships.
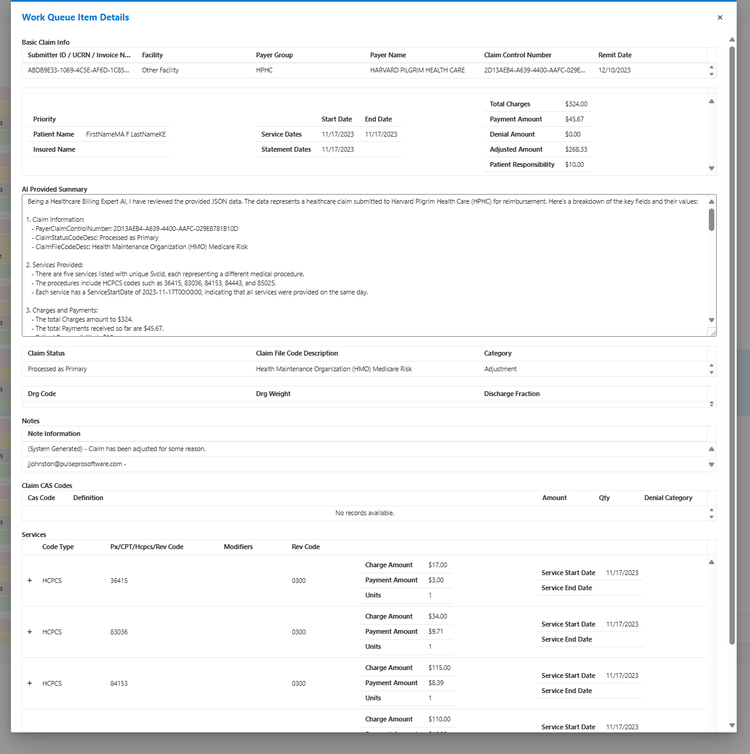
AI-generated summaries provide faster decision-making capabilities, while smart work queues streamline your team's workflow. Track KPIs including collection ratios, resubmissions, and comprehensive revenue integrity metrics.
ROOT CAUSE ANALYSIS
Capability: Integrated Problem-Solving
Method: Trend Identification & Resolution
Result: Long-Term Denial Prevention
What sets Revenue Navigator apart is its seamless integration with MRSAuditQ. Send trending denials directly to MRSAuditQ to identify and resolve root causes, ensuring long-term improvements and reducing future denials across your entire organization.
Perform comprehensive root cause analyses, review and track payment posting, and evaluate payments made on claims. This integrated approach provides a complete payment review and tracking system that maintains high standards of revenue integrity while ensuring environmental sustainability in your revenue cycle.

What Makes revenue navigator Different?
The Denial Epidemic
Medical denials in the United States have surged to a staggering $20 billion annually. These denials represent lost revenue opportunities that can significantly impact your healthcare organization's financial health.
Increase Revenue Potential
Our solution has the potential to generate an increase in revenue of hundreds of thousands of dollars over the next 12 months. Revenue Navigator not only recovers lost revenue but also provides insights to help negotiate better contracts with insurance providers based on denial patterns.
Efficient Denial Management
Revenue Navigator is designed to help healthcare organizations seize opportunities hidden within reimbursement obstacles. Our advanced denial management solution efficiently identifies, analyzes, and resolves denied claims.
Enhance Operational Efficiency
Revenue Navigator simplifies your denial management process, allowing your team to address denials promptly and accurately. Plus, with our unique integration, you can send trending denials to MRSAuditQ to identify and resolve the root causes, setting us apart from the competition.
Integration with MRSAuditQ
What sets Revenue Navigator apart is its seamless integration with MRSAuditQ. Send trending denials directly to MRSAuditQ to resolve root causes, ensuring long-term improvements and reducing future denials.
Reclaim Lost Revenue. Prevent Future Denials.
valuable insights
Denial Management
Monitor Payer Performance and Payment Performance
Perform Root Cause Analyses
Review and Track Payment Posting and Evaluation of Payments made on claims!
Payment Review and Tracking Posting
Denial and Revenue KPIs
REVENUE INTEGRITY
work queues

READY TO RECOVER LOST REVENUE?
SCHEDULE A DEMO TODAY AND DISCOVER HOW REVENUE NAVIGATOR CAN TRANSFORM YOUR DENIAL MANAGEMENT